When we talk about conditions that affect how our bodies work, particularly how our brain and spinal cord communicate with everything else, it can feel a bit overwhelming, you know? But sometimes, just learning a little about what's going on can make a big difference. One such condition, often called .ms for short, involves the body's own defense system mistakenly targeting something really important.
This particular condition, .ms, is about a kind of wearing away of the protective covering that surrounds our nerve fibers. Think of it like the insulation around an electrical wire; when that insulation gets damaged, the signals don't travel as smoothly, or perhaps not at all. This can lead to a whole range of experiences for someone, and it's quite unique to each person, more or less.
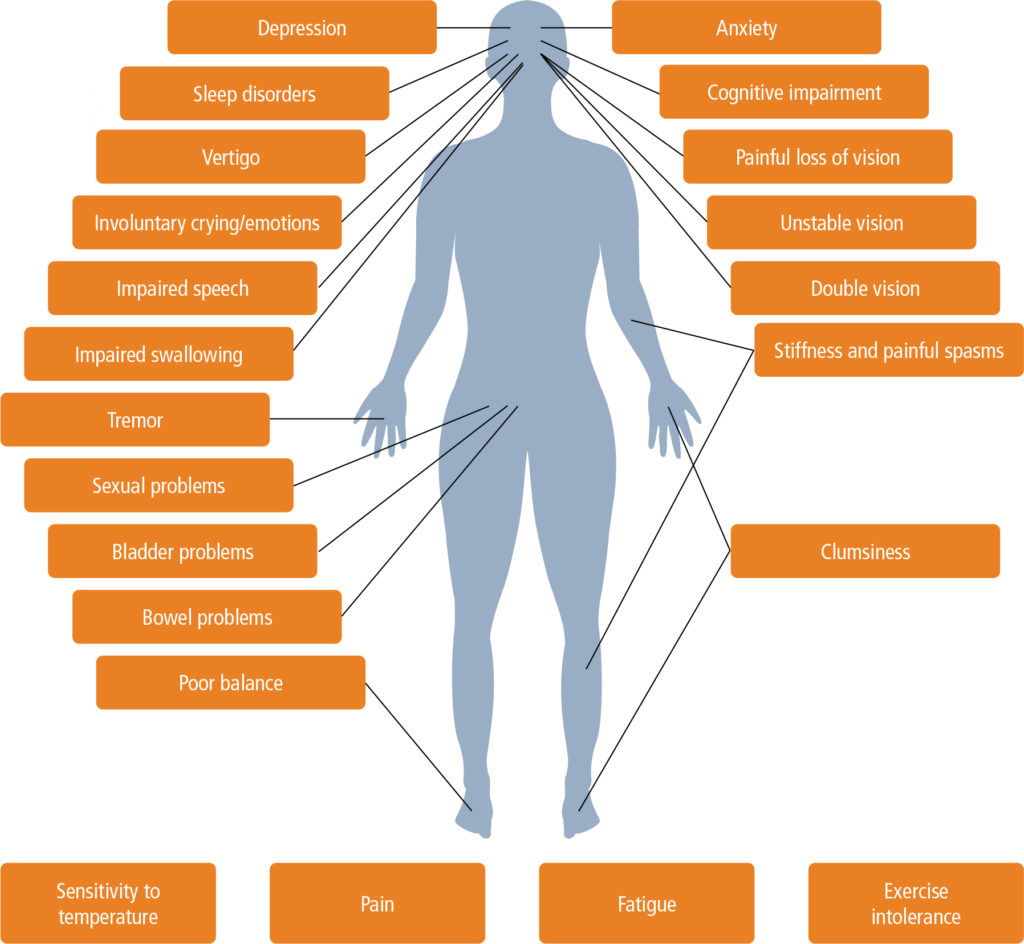
So, because these messages from the brain and spinal cord might not get where they need to go, people living with .ms can experience various things. These can include feelings of numbness, a certain weakness in parts of the body, sometimes difficulty with walking, and even changes in how they see the world. It’s a condition that shows up differently for different people, in a way.
Table of Contents
- What is .ms, really?
- How does .ms affect the body?
- Are there specific tests for .ms?
- What about Secondary Progressive .ms?
- How is .ms treated?
- What about everyday living with .ms?
- Is there a link between .ms and other conditions?
- Where can people find good support for .ms?
What is .ms, really?
At its heart, .ms is a condition where the body's own immune system, which is usually there to protect us from outside invaders, gets a little confused. It starts to attack the protective layer that wraps around the nerves in your brain and spinal cord. This layer has a name, myelin, and it's super important for helping nerve signals move quickly and smoothly, you know? When this myelin gets damaged, those signals can slow down or even stop, causing a variety of physical effects.
This kind of condition, where the immune system turns on itself, is sometimes called an autoimmune disease. It means your body is essentially seeing its own healthy parts as something harmful. For people with .ms, this means the myelin, which is like the insulation on electrical wiring for your body's communication system, gets worn away or broken down. This can affect how your brain talks to the rest of your body, which is pretty important, as a matter of fact.
The central nervous system, which includes the brain and spinal cord, is where all these messages are sent and received. When .ms affects this system, it's considered the most common condition of its kind that causes this sort of demyelination, or the loss of that protective coating. It's a bit like having a busy phone line where the connection keeps getting fuzzy or dropping out, so signals don't get through clearly, or so it seems.
How does .ms affect the body?
Because .ms messes with the way nerve signals travel, it can lead to a whole bunch of different physical experiences. One common thing people talk about is numbness, a feeling like a part of your body has fallen asleep, but it might not go away. Then there's weakness, where muscles just don't seem to have the same strength they used to, which can be quite noticeable, you know?
Walking can become a real challenge for some, as the signals telling legs and feet what to do might get mixed up or delayed. This can make balance tricky and movement feel very different. And then there are vision changes; sometimes people experience blurry vision, double vision, or even a temporary loss of sight in one eye, which is rather disorienting.
These effects happen because the damaged myelin means the electrical impulses from the brain aren't reaching their destinations effectively. So, if your brain tells your leg to move, that message might not get through clearly, or it might get there slowly. This is why things like physical movement and even just feeling sensations can be impacted, as I was saying.
Are there specific tests for .ms?
One of the tricky things about .ms is that there isn't just one single test that can tell someone they have it. It's not like a blood test for cholesterol, for example, where a number tells you everything. Instead, doctors have to piece together a picture from several different sources to figure out if someone has .ms, which can make the process a bit drawn out, you know?
The process usually starts with a detailed chat about your medical background, going over any symptoms you've been experiencing and when they started. Then there's a physical examination, where a doctor will check things like your reflexes, balance, and coordination. These steps give them clues about how your nervous system might be working, or not working, in some respects.
Beyond that, doctors often use special scans called MRIs, which are like very detailed pictures of your brain and spinal cord. These scans can show areas where the myelin might be damaged. Sometimes, they also do a spinal tap, which involves collecting a small amount of fluid from around your spinal cord to look for certain markers. It's a combination of all these pieces of information that helps a doctor make a proper determination, or so it seems.
What about Secondary Progressive .ms?
For some people who have a type of .ms that involves periods of symptoms followed by times when things feel better, there's another pattern that can sometimes develop. This is called secondary progressive .ms, or SPMS. It means that after a period of those ups and downs, the symptoms might start to get steadily worse over time, which can be a difficult shift, you know?
This progression of symptoms can happen gradually, sometimes over many years, perhaps ten to forty years after the first signs of .ms appeared. It's important to remember that this doesn't happen to everyone with .ms; it's seen in about twenty to forty percent of people who initially have the relapsing-remitting form. The progression can happen with or without those periods of feeling better, or so it seems.
Research into how this progressive form of .ms develops has often focused on changes happening within the brain tissue itself. This helps medical professionals get a better grip on what's happening at a deeper level and, hopefully, figure out ways to help. It's a continuous area of study, as a matter of fact, trying to learn more about how this condition changes over time.
How is .ms treated?
It's important to know that right now, there isn't a way to completely get rid of .ms. There's no cure that makes it disappear for good. However, that doesn't mean there's nothing that can be done. Treatment for .ms usually focuses on several key areas, aiming to help people manage the condition and live as well as they can, you know?
One main goal of treatment is to help people recover more quickly from those times when symptoms flare up, often called attacks or relapses. Another focus is on trying to reduce how often these relapses happen. And a very big part of the treatment picture is working to slow down the overall progression of the condition, trying to keep it from getting worse too quickly, which is pretty important.
Beyond those broader goals, a lot of the care for .ms is about making everyday life easier by helping with the symptoms. This often includes things like physical therapy, which helps people keep their strength and movement, and occupational therapy, which helps them find ways to do daily activities more independently. These therapies are very practical and help people maintain their usual routines, or so it seems.
What about everyday living with .ms?
Living with .ms means learning to adapt and find strategies that work for you. Since the condition can affect things like movement and sensation, physical therapy can be a really helpful tool. It involves exercises and activities designed to keep muscles strong and flexible, which can make a big difference in maintaining independence, you know?
Occupational therapy is another wonderful resource. This kind of therapy helps people figure out different ways to do daily tasks, whether it's getting dressed, cooking, or managing personal care. It's about finding practical solutions and adapting routines so that people can continue to do the things that matter to them, which is quite empowering, as a matter of fact.
These therapies are a core part of managing the day-to-day effects of .ms. They're not just about fixing things, but about helping people live their lives fully, even with the challenges the condition might present. It's about building resilience and finding smart ways to navigate daily activities, so that life can be as fulfilling as possible, you know?
Is there a link between .ms and other conditions?
It's interesting to consider how .ms might connect with other health conditions. Sometimes, when one part of the body's system is affected, it can have ripple effects elsewhere. For example, there's been some talk about a connection between .ms and something called epilepsy, which involves seizures. It's a question that people often ask, you know?
What we've seen is that people who have .ms do tend to experience epileptic seizures more often than people who don't have .ms. This doesn't mean that everyone with .ms will have seizures, but the chances are somewhat higher. It's another aspect that medical professionals consider when they're looking at the full picture of someone's health, as a matter of fact.
This kind of observation helps researchers and doctors learn more about the broader impact of .ms on the body's systems. It highlights how complex the human body is and how different conditions can sometimes influence each other. So, while it's not a direct cause-and-effect in every person, it's a link that's been noted, and it's quite interesting, you know?
Where can people find good support for .ms?
When it comes to getting good support and care for .ms, finding specialists who truly focus on this condition can make a big difference. Places like the Mayo Clinic, for instance, have teams that see thousands of people with .ms every year. Their concentration on this specific condition means they build up a lot of experience and a deep sort of understanding, you know?
Having medical teams with this kind of focused knowledge means they're very familiar with the different ways .ms can show up and how it can progress. This experience helps them to offer care that's really well-informed and suited to each person's unique situation. It's about getting care from people who have seen a lot of different cases and have a lot of practical wisdom, as a matter of fact.
So, for anyone looking for help or information about .ms, seeking out medical centers or specialists who have a strong background and focus in this area can be very helpful. They are often at the forefront of learning more about the condition and how to best support people living with it, which is pretty reassuring, you know?
Related Resources:


Detail Author:
- Name : Lue Haag
- Username : lang.garth
- Email : charles.runte@yahoo.com
- Birthdate : 1982-12-17
- Address : 9934 Ford Radial Apt. 552 Lake Jacquesborough, KS 46991-7591
- Phone : 801-874-9047
- Company : Volkman-Quitzon
- Job : Medical Equipment Repairer
- Bio : Rerum ut explicabo quisquam omnis. Exercitationem numquam velit ut sint distinctio ut. Autem eos consectetur ullam in quia autem. Itaque totam ullam qui quod rerum perferendis odit sapiente.
Socials
twitter:
- url : https://twitter.com/magdalena_stehr
- username : magdalena_stehr
- bio : Dolores molestiae architecto aut consequatur. Quas voluptate natus consequatur enim nostrum vitae. Officiis aliquam soluta tempore.
- followers : 2704
- following : 210
instagram:
- url : https://instagram.com/stehrm
- username : stehrm
- bio : Omnis ipsum harum tempore. Reiciendis earum impedit veniam sint porro optio quia.
- followers : 544
- following : 187
tiktok:
- url : https://tiktok.com/@magdalena5014
- username : magdalena5014
- bio : Adipisci recusandae sit quaerat quia.
- followers : 1053
- following : 68