Multiple Sclerosis, often abbreviated as MS, is a complex and unpredictable neurological condition that affects millions worldwide. It's a disease where the body's own immune system mistakenly attacks the protective covering of nerves, leading to a wide array of symptoms and challenges. Understanding MS is the first step towards managing its impact and supporting those who live with it.
This comprehensive guide delves into the intricacies of Multiple Sclerosis, from its fundamental nature and diverse symptoms to the diagnostic journey and the ongoing efforts in research and treatment. Our aim is to provide clear, authoritative, and trustworthy information, empowering readers with knowledge about this significant health condition.
Table of Contents
- What is Multiple Sclerosis (MS)?
- The Unseen Battle: Symptoms of MS
- Diagnosing MS: A Complex Puzzle
- Types and Progression of MS
- Living with MS: Management and Treatment
- MS and Co-occurring Conditions: The Link with Epilepsy
- Research and Future Directions in MS
- Empowering Yourself: Resources and Support for MS Patients
What is Multiple Sclerosis (MS)?
At its core, Multiple Sclerosis is a chronic, often progressive, disease of the central nervous system (CNS), which includes the brain, spinal cord, and optic nerves. It is the most common demyelinating disease of the central nervous system. In this disease, the immune system attacks the myelin sheath, or the cells that produce it. The myelin sheath is a fatty, protective covering that insulates nerve fibers, much like the insulation around an electrical wire. This covering is crucial for the rapid and efficient transmission of electrical signals (nerve impulses) throughout the body.
When the immune system launches an assault on this vital covering, it leads to inflammation and damage, causing the myelin to break down. This process, known as demyelination, disrupts the flow of information between the brain and the rest of the body. The resulting "short circuits" or blockages in nerve communication are responsible for the diverse range of symptoms experienced by individuals with MS. The damage can also extend to the underlying nerve fibers themselves, leading to more permanent disability. While the exact cause of why the immune system turns against its own tissues remains unknown, it is believed to be a combination of genetic predisposition and environmental factors.
The Unseen Battle: Symptoms of MS
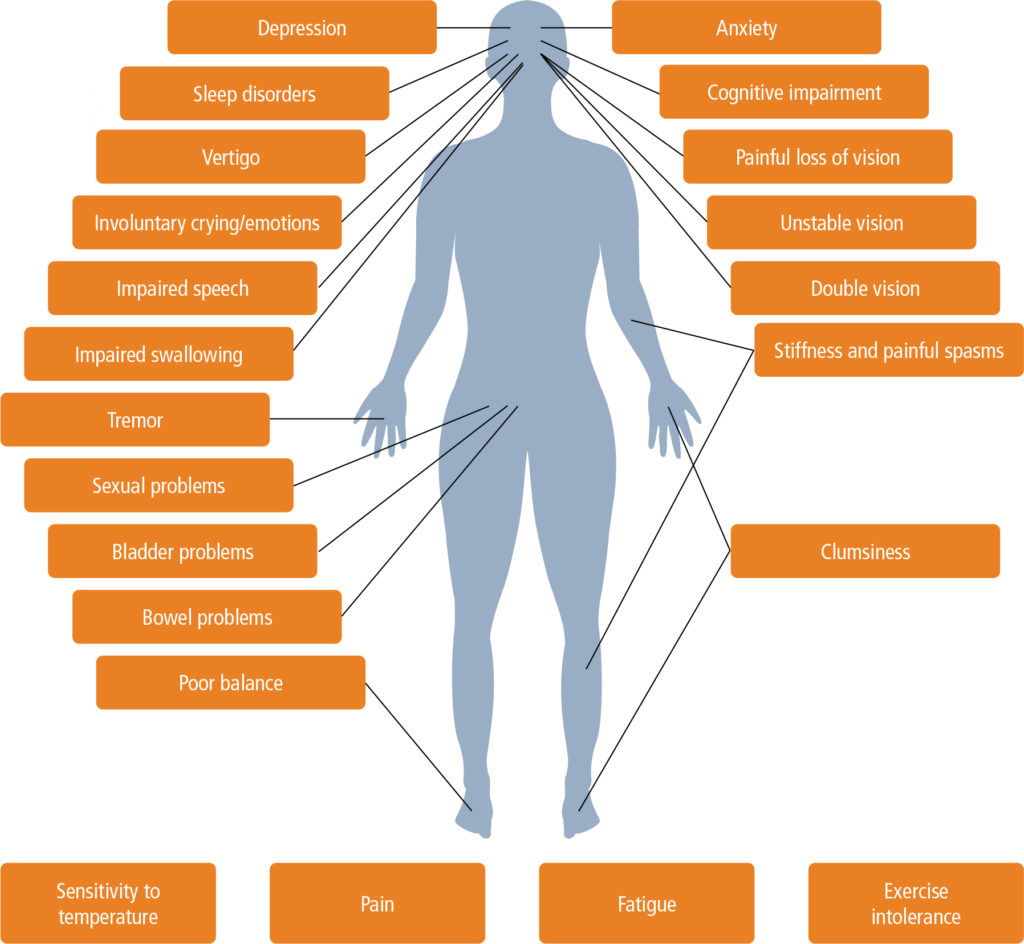
The symptoms of Multiple Sclerosis are incredibly varied and unpredictable, depending on which part of the central nervous system is affected and the extent of the damage. No two people with MS will experience the exact same set of symptoms, and symptoms can fluctuate over time, appearing and disappearing, or worsening. This unpredictability is one of the most challenging aspects of living with the condition.
Common early symptoms often include sensory disturbances. For instance, Multiple Sclerosis can cause numbness, a tingling sensation, or even a feeling of "pins and needles" in the limbs, face, or trunk. Weakness is another frequent symptom, affecting one or more limbs, making everyday tasks difficult. Trouble walking, often due to muscle weakness, spasticity (muscle stiffness), or problems with balance and coordination, is a hallmark of the disease. Vision changes are also very common and can be among the first noticeable symptoms. These might include blurred vision, double vision, or even temporary loss of vision in one eye, often accompanied by pain during eye movement.
- Ash Trevino Flash Santos Twitter
- Lucy Mochi Feet
- Aire Jay Twitter
- Luna Bella Twiter
- Baby Gemini Swallowed
Beyond these primary symptoms, individuals with MS may also experience chronic fatigue, which is often debilitating and disproportionate to activity levels. Cognitive issues, such as problems with memory, attention, and processing speed, can also occur. Other symptoms can include dizziness, vertigo, bladder and bowel dysfunction, pain, depression, and sexual dysfunction. The cumulative effect of these symptoms can significantly impact a person's quality of life, making early diagnosis and management crucial.
Diagnosing MS: A Complex Puzzle
Diagnosing Multiple Sclerosis can be a challenging and lengthy process because there are no specific tests for MS that definitively confirm the condition on their own. Instead, the diagnosis is given by a combination of factors, requiring a thorough evaluation by a neurologist. This comprehensive approach is necessary to rule out other conditions that might mimic MS symptoms and to confirm the presence of characteristic MS lesions in the central nervous system.
The diagnostic journey typically begins with a detailed medical history. The doctor will ask about the patient's symptoms, when they started, how they have progressed, and any previous neurological events. This is followed by a comprehensive physical exam, where the neurologist assesses neurological function, including reflexes, coordination, balance, vision, and sensation. A diagnosis of multiple sclerosis also involves demonstrating evidence of demyelination in at least two separate areas of the central nervous system at two different points in time, or evidence of ongoing disease activity.
The Role of MRI in MS Diagnosis
Magnetic Resonance Imaging (MRI) is a cornerstone of MS diagnosis. MRI scans of the brain and spinal cord are highly sensitive in detecting the characteristic lesions (areas of demyelination and damage) that are indicative of Multiple Sclerosis. These lesions appear as bright spots on the MRI and can be seen in different locations, such as the white matter of the brain, brainstem, cerebellum, and spinal cord. The presence of lesions in different areas and at different times (dissemination in space and time) helps to meet the diagnostic criteria for MS. Sometimes, a contrast dye (gadolinium) is injected during the MRI to highlight active inflammation, indicating new or recently active lesions.
Spinal Tap: Unveiling Clues
A spinal tap, also known as a lumbar puncture, is another important diagnostic tool for MS. During this procedure, a small amount of cerebrospinal fluid (CSF) is collected from the spinal canal. The CSF is then analyzed for specific markers that are often found in people with Multiple Sclerosis. These markers include oligoclonal bands (OCBs), which are specific proteins that indicate inflammation in the central nervous system, and an elevated IgG index, which points to increased antibody production within the CNS. While not all individuals with MS will have these CSF abnormalities, their presence strongly supports a diagnosis of MS, especially when combined with clinical symptoms and MRI findings.
Types and Progression of MS
Multiple Sclerosis manifests in several forms, each with its own pattern of progression. Understanding these types is crucial for both diagnosis and treatment planning. The most common form, affecting about 85% of people initially, is Relapsing-Remitting MS (RRMS). In RRMS, individuals experience clearly defined attacks (relapses) of new or worsening neurological symptoms, followed by periods of partial or complete recovery (remissions). During remissions, symptoms may disappear entirely or significantly improve, though some residual deficits might remain.
Another type is Primary Progressive MS (PPMS), which affects about 10-15% of people with MS. In PPMS, there is a gradual, steady accumulation of disability from the onset, without distinct relapses or remissions. Symptoms slowly worsen over time, though the rate of progression can vary among individuals.
Secondary Progressive Multiple Sclerosis (SPMS)
Secondary Progressive Multiple Sclerosis (SPMS) is a form of the disease that often develops after an initial period of Relapsing-Remitting MS. As stated in the provided data, "التصلب المتعدد المتفاقم الثانوي يصاب 20% إلى 40% من مرضى التصلب المتعدد المنتكس-المهتدئ بتقدم مُطرد للأعراض مع مرور الوقت. وقد يحدث هذا التقدم مع فترات من الهَدْأَة أو من دونها ويحدث في غضون 10 أعوام إلى 40 عامًا من بداية..." This translates to: "Secondary Progressive Multiple Sclerosis affects 20% to 40% of relapsing-remitting MS patients with a steady progression of symptoms over time. This progression may occur with or without periods of remission and typically happens within 10 to 40 years from the onset..."
This transition to SPMS means that after years of relapses and remissions, the disease begins to progress more steadily, with a gradual worsening of neurological function and increasing disability, independent of relapses. While some individuals might still experience occasional relapses during the SPMS phase, the defining characteristic is the continuous accumulation of disability. The shift to SPMS can significantly impact a person's life, necessitating a re-evaluation of treatment strategies and support systems.
Living with MS: Management and Treatment
While there is currently no cure for Multiple Sclerosis, significant advancements in treatment have transformed the outlook for many individuals living with the condition. The primary goals of MS management are to slow disease progression, reduce the frequency and severity of relapses, manage symptoms, and improve quality of life. Treatment strategies are highly individualized, tailored to the specific type of MS, the severity of symptoms, and the patient's overall health.
Disease-modifying therapies (DMTs) are a cornerstone of MS treatment, particularly for relapsing forms of MS. These medications work by altering the immune system to reduce the frequency and severity of relapses and to slow the accumulation of disability. DMTs are administered in various ways, including injections, oral medications, and intravenous infusions. The choice of DMT depends on many factors, including efficacy, safety profile, and patient preference.
In addition to DMTs, symptom management is a critical component of living with MS. Medications can help alleviate specific symptoms such as fatigue, spasticity, pain, bladder problems, and depression. Rehabilitation therapies, including physical therapy, occupational therapy, and speech therapy, play a vital role in helping individuals maintain function, improve mobility, manage daily tasks, and adapt to new challenges. Lifestyle adjustments, such as regular exercise, a healthy diet, stress management, and avoiding overheating, can also contribute to overall well-being. Regular monitoring by a neurologist, often involving periodic MRI scans and neurological exams, is essential to track disease activity and adjust treatment as needed.
MS and Co-occurring Conditions: The Link with Epilepsy
Living with Multiple Sclerosis can often involve managing co-occurring conditions, which are health issues that appear alongside MS. These comorbidities can complicate the disease course and impact quality of life. One such condition that has a notable connection with MS is epilepsy. The question "Is there any connection between multiple sclerosis and epilepsy?" is often raised by patients and clinicians alike.
Research indicates that epileptic seizures are more common in people who have Multiple Sclerosis (MS) than in those who don't have MS. While the exact reasons for this increased prevalence are still being investigated, it is believed that the brain lesions caused by MS, particularly those located in the cerebral cortex, can disrupt normal electrical activity in the brain, leading to seizures. The inflammation and scarring associated with MS can create an environment that predisposes individuals to epilepsy.
Seizures in MS patients can vary in type and severity, ranging from focal seizures that affect a specific part of the brain to generalized seizures that affect both sides of the brain. Managing epilepsy in the context of MS often requires careful collaboration between neurologists specializing in MS and those specializing in epilepsy. Treatment typically involves anti-epileptic medications, chosen to minimize interactions with MS treatments and to manage both conditions effectively. Recognizing this potential link is important for comprehensive care and for addressing all aspects of a person's health when living with MS.
Research and Future Directions in MS
The field of Multiple Sclerosis research is dynamic and constantly evolving, bringing new hope for improved treatments and, ultimately, a cure. Scientists worldwide are tirelessly working to unravel the mysteries of MS, from understanding its underlying causes to developing more effective therapies. Studies of the development of progressive multiple sclerosis (MS) have focused mostly on brain parenchymal changes. This area of research is crucial because it investigates the damage to the actual nerve tissue (parenchyma) of the brain, not just the myelin, which is believed to be a key driver of irreversible disability in progressive forms of MS.
Current research avenues include exploring neuroprotection strategies to prevent nerve damage, remyelination approaches to repair damaged myelin, and new immunomodulatory drugs that can more precisely target the immune system without causing broad suppression. Genetic studies are helping to identify risk factors, while advanced imaging techniques are providing a deeper insight into disease activity and progression. The goal is not only to halt the disease but also to reverse its effects and restore lost function. Continued investment in research and clinical trials is vital to accelerate these discoveries and bring them from the lab to patients.
Empowering Yourself: Resources and Support for MS Patients
For individuals diagnosed with Multiple Sclerosis and their families, navigating the complexities of the disease can be overwhelming. However, a wealth of resources and support systems are available to help. Understanding the basics of multiple sclerosis is the first step, and reputable organizations and medical institutions are invaluable sources of information. For instance, you can watch as a Mayo Clinic expert explains the basics of multiple sclerosis, providing clear and concise insights into the condition. Such expert explanations help demystify the disease and provide a foundational understanding.
Beyond initial understanding, it's crucial to find out about multiple sclerosis symptoms, causes, prevention, diagnosis and treatment from reliable sources. National MS societies and foundations offer comprehensive information, educational programs, and support groups where individuals can connect with others facing similar challenges. These communities provide emotional support, practical advice, and a sense of belonging. Healthcare teams, including neurologists, nurses, therapists, and social workers, are also critical resources, offering personalized care plans and guidance. Empowering yourself with knowledge and connecting with support networks can significantly improve the journey of living with MS, fostering resilience and promoting a better quality of life.
Conclusion
Multiple Sclerosis (MS) is a chronic and often unpredictable neurological condition that impacts millions globally. As we've explored, it's a disease where the immune system attacks the protective myelin sheath around nerves, leading to a diverse range of symptoms from numbness and weakness to vision changes and trouble walking. Diagnosing MS is a multi-faceted process involving medical history, physical exams, MRI scans, and sometimes spinal tap results, as there's no single definitive test. We've also touched upon the different types of MS, including the progression to Secondary Progressive MS, and the importance of ongoing research into areas like brain parenchymal changes and the link between MS and conditions like epilepsy.
While living with MS presents unique challenges, significant advancements in treatment and management offer hope and improved quality of life. Understanding this complex condition is paramount for both those directly affected and their support networks. We encourage you to continue seeking knowledge from trusted sources, engage with healthcare professionals, and connect with supportive communities. If you or a loved one are navigating an MS diagnosis, remember that information is power. Share this article to spread awareness and understanding, and consider exploring more resources from reputable organizations to empower your journey with MS. Your insights and experiences are valuable—feel free to leave a comment below and share your thoughts.
Related Resources:


Detail Author:
- Name : Miss Claudine Walker III
- Username : gabriella.olson
- Email : lulu33@yahoo.com
- Birthdate : 1970-03-16
- Address : 21827 Frank Fords Suite 521 Port Rickview, OK 57311
- Phone : 754.791.8554
- Company : Lemke, Bartoletti and Weissnat
- Job : Lathe Operator
- Bio : Et assumenda praesentium vero ex at. Et eaque doloribus magnam libero quidem iste. Doloribus officia id incidunt quia aut facilis sed.
Socials
linkedin:
- url : https://linkedin.com/in/euna.veum
- username : euna.veum
- bio : Iste sit quidem exercitationem quo.
- followers : 1769
- following : 1409
instagram:
- url : https://instagram.com/euna796
- username : euna796
- bio : Soluta blanditiis assumenda amet praesentium aperiam sed. Quia hic odit molestias.
- followers : 3345
- following : 1450