Multiple Sclerosis (MS) is a complex neurological condition that affects millions worldwide, often presenting with a wide array of symptoms that can significantly impact daily life. This chronic disease, which primarily targets the central nervous system, can be challenging to diagnose and manage, yet advancements in medical research offer increasing hope and improved quality of life for those affected. Understanding the intricacies of MS is crucial for patients, caregivers, and the general public to foster awareness, support, and effective management strategies.
This article delves deep into the nature of Multiple Sclerosis, exploring its causes, diverse symptoms, diagnostic processes, and the latest treatment options. We aim to provide a comprehensive, easy-to-understand guide that adheres to the principles of E-E-A-T (Expertise, Authoritativeness, Trustworthiness) and YMYL (Your Money or Your Life) by relying on established medical knowledge and reputable sources, such as insights from Mayo Clinic experts. Our goal is to empower readers with accurate information, helping them navigate the complexities of this condition.
Table of Contents
- Understanding Multiple Sclerosis (MS)
- Common Symptoms of Multiple Sclerosis
- Diagnosing Multiple Sclerosis: A Complex Puzzle
- The Various Clinical Courses of Multiple Sclerosis
- Current Treatments and Hope for MS Patients
- Living with an MS Diagnosis
- Research and the Future Outlook for Multiple Sclerosis
- The Importance of Early Intervention in MS
Understanding Multiple Sclerosis (MS)
Multiple Sclerosis, often referred to simply as MS, is a chronic autoimmune disease that affects the brain and spinal cord, which together form the central nervous system. It's a condition where the body's own immune system mistakenly attacks the protective covering of nerves. This covering, called the myelin sheath, is crucial for the rapid and efficient transmission of electrical signals throughout the nervous system. When this myelin is damaged, nerve signals can be slowed down, distorted, or even completely blocked, leading to a wide range of symptoms.
What is MS?
At its core, Multiple Sclerosis is a disease that causes the breakdown of the protective covering of nerves. This process is known as demyelination. Think of your nerves like electrical wires, and myelin as the insulation around them. Just as damaged insulation can cause electrical shorts or failures, damage to myelin in MS disrupts the normal flow of nerve impulses. This damage can occur in various parts of the brain, optic nerves, and spinal cord, which explains the diverse symptoms experienced by individuals with the condition. The exact cause of MS is still unknown, but it is believed to involve a combination of genetic predisposition and environmental factors.
The Immune System's Attack
In Multiple Sclerosis, the immune system, which is designed to protect the body from foreign invaders like bacteria and viruses, mistakenly identifies myelin as a threat. This leads to an inflammatory response where immune cells attack and destroy the myelin. Over time, this chronic inflammation can also lead to nerve damage itself. The unpredictable nature of these attacks and the varied locations of lesions (areas of damage) in the central nervous system make MS a highly individualized disease, meaning no two people will experience it in exactly the same way. The progression and severity of symptoms can vary greatly, even within the same individual over time.
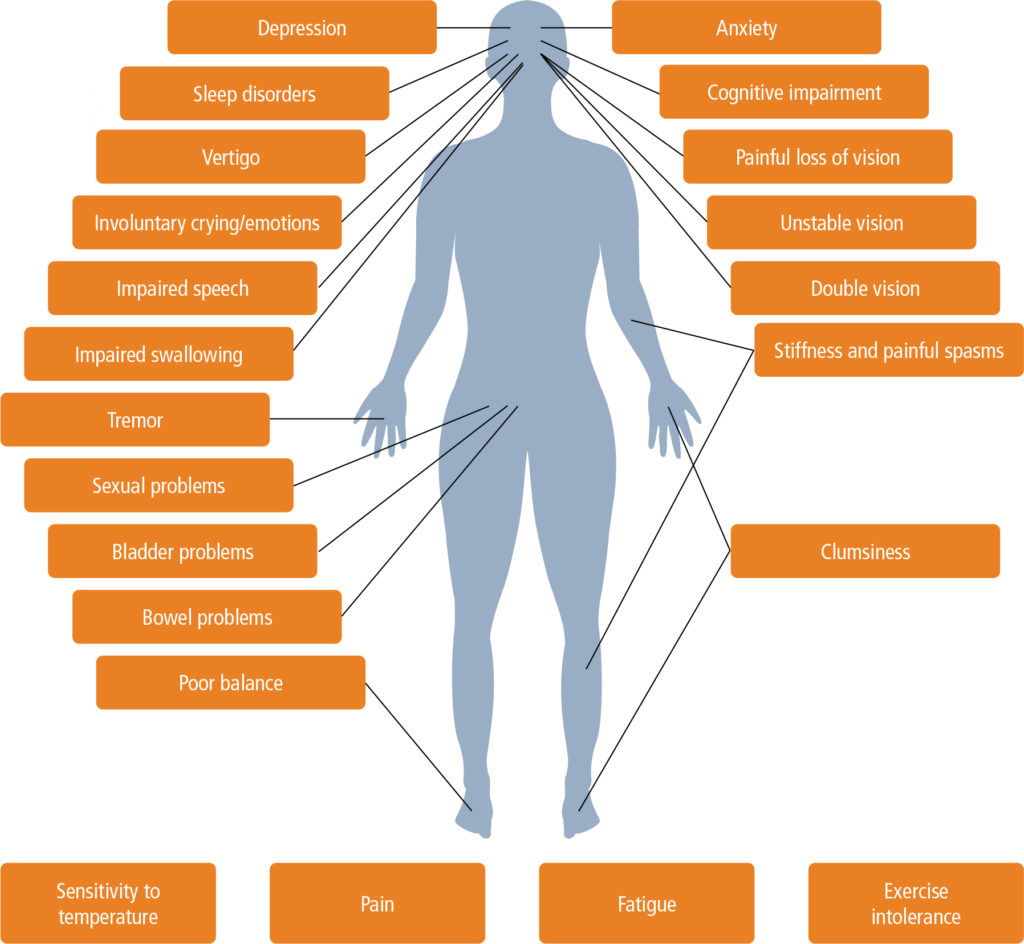
Common Symptoms of Multiple Sclerosis
The symptoms of Multiple Sclerosis are as varied as the individuals who experience them, largely depending on which nerves are affected and the extent of the damage. Because MS can impact any part of the central nervous system, the symptoms can range from mild and transient to severe and debilitating. Recognizing these symptoms is often the first step towards seeking a diagnosis and managing the condition.
Neurological Manifestations
Multiple Sclerosis can cause a wide array of neurological symptoms. Common early signs often include:
- Numbness and Weakness: One of the most frequently reported symptoms is numbness or tingling sensations, often described as pins and needles, in the limbs or face. This can be accompanied by muscle weakness, making everyday tasks challenging.
- Fatigue: Overwhelming fatigue, disproportionate to activity levels, is a pervasive symptom of MS. It's not just ordinary tiredness but a profound exhaustion that can interfere with work, social activities, and daily routines.
- Pain: Chronic pain, including neuropathic pain (nerve pain) and musculoskeletal pain, is common in MS.
- Cognitive Changes: Many people with MS experience "brain fog," which can manifest as problems with memory, attention, information processing, and problem-solving.
- Speech and Swallowing Difficulties: Dysarthria (slurred speech) and dysphagia (difficulty swallowing) can occur due to nerve damage affecting the muscles involved in these functions.
- Bladder and Bowel Problems: Bladder dysfunction (e.g., frequent urination, urgency, incontinence) and bowel issues (e.g., constipation) are common and can significantly impact quality of life.
Vision and Mobility Challenges
Beyond general neurological symptoms, Multiple Sclerosis frequently affects vision and mobility, leading to specific challenges:
- Vision Changes: Vision problems are often among the first symptoms of MS. These can include:
- Blurred vision
- Double vision (diplopia)
- Partial or complete loss of vision, usually in one eye at a time, often accompanied by pain during eye movement (optic neuritis).
- Trouble Walking: Mobility issues are a hallmark of MS. This can manifest as:
- Balance problems (ataxia)
- Gait difficulties, leading to an unsteady or dragging walk
- Muscle spasticity (stiffness and involuntary muscle spasms)
- Weakness in the legs, making it difficult to lift the feet or maintain balance.
These symptoms can fluctuate in intensity and may come and go, especially in the early stages of the disease.
Diagnosing Multiple Sclerosis: A Complex Puzzle
Diagnosing Multiple Sclerosis can be a challenging and lengthy process because there are no specific tests for MS that definitively confirm the condition with a single result. Instead, the diagnosis is given by a combination of factors, creating a comprehensive picture of the patient's health. This diagnostic journey often involves ruling out other conditions that might present with similar symptoms.
A diagnosis of Multiple Sclerosis typically involves:
- Medical History: A thorough review of the patient's symptoms, their onset, progression, and any previous neurological events. This helps the neurologist understand the pattern of attacks and remissions.
- Physical Exam: A detailed neurological examination to assess reflexes, muscle strength, coordination, balance, sensation, and vision. This helps identify signs of nerve damage consistent with MS.
- MRIs (Magnetic Resonance Imaging): MRIs of the brain and spinal cord are crucial. They can reveal lesions (areas of damage or inflammation) in the central nervous system that are characteristic of MS. The presence of lesions in different areas of the brain or spinal cord, or lesions that have developed at different times, provides strong evidence for a diagnosis of Multiple Sclerosis.
- Spinal Tap (Lumbar Puncture) Results: A spinal tap involves collecting a sample of cerebrospinal fluid (CSF) from the spinal canal. This fluid is then analyzed for abnormalities, such as the presence of oligoclonal bands (proteins that indicate inflammation in the central nervous system), which are found in a high percentage of people with MS.
- Evoked Potentials: These tests measure the electrical activity of the brain in response to sensory stimulation (visual, auditory, or somatosensory). They can detect slowed nerve conduction in pathways affected by MS, even if the patient doesn't report symptoms in those areas.
The diagnostic criteria for MS, such as the revised McDonald criteria, require evidence of demyelination in at least two different areas of the central nervous system at two different points in time, or evidence of dissemination in space and time. This systematic approach ensures an accurate diagnosis of Multiple Sclerosis, distinguishing it from other neurological conditions.
The Various Clinical Courses of Multiple Sclerosis
Multiple Sclerosis is not a single, uniform disease; rather, it manifests in several distinct clinical courses, each with its own pattern of symptom progression. Understanding these courses is vital for prognosis and treatment planning. By far the most common form of MS is Relapsing-Remitting MS (RRMS).
- Relapsing-Remitting MS (RRMS): This is the most common form, affecting about 85% of people diagnosed with MS initially. RRMS is characterized by clearly defined attacks (relapses or exacerbations) of new or worsening neurological symptoms, followed by periods of partial or complete recovery (remissions). During remissions, symptoms may disappear entirely, or some symptoms may persist but do not worsen. The disease does not progress during the remission periods.
- Secondary Progressive MS (SPMS): This course typically follows an initial period of RRMS. In SPMS, the disease begins to progress more steadily, with a gradual worsening of neurological function over time, independent of relapses. This progression may or may not include occasional relapses, minor remissions, or plateaus. The "Data Kalimat" notes that 20% to 40% of patients with relapsing-remitting multiple sclerosis develop a steady progression of symptoms over time. This progression may occur with or without periods of remission and occurs within 10 to 40 years from the onset of the disease. Studies of the development of progressive Multiple Sclerosis (MS) have focused mostly on brain parenchymal changes, highlighting the underlying neurological shifts.
- Primary Progressive MS (PPMS): Affecting about 15% of people with MS, PPMS is characterized by a gradual, steady accumulation of disability from the onset, without early relapses or remissions. There may be temporary plateaus or minor improvements, but the disease generally continues to worsen over time.
- Progressive-Relapsing MS (PRMS): This is the least common course, characterized by a steady neurological decline from the onset, with superimposed acute attacks.
Each course of Multiple Sclerosis presents unique challenges and requires tailored management strategies. Regular monitoring and communication with healthcare providers are essential to adapt treatment plans as the disease course evolves.
Current Treatments and Hope for MS Patients
While there is no cure for Multiple Sclerosis (MS) currently, significant advancements in drug development have transformed the landscape of MS treatment. The goal of treatment is to manage symptoms, reduce the frequency and severity of relapses, slow disease progression, and improve quality of life. The "Data Kalimat" acknowledges this, stating, "There is no cure for Multiple Sclerosis (MS). However, new drug development activities for its treatment have made some progress."
Treatment strategies for Multiple Sclerosis typically fall into several categories:
- Disease-Modifying Therapies (DMTs): These medications are the cornerstone of MS treatment, particularly for relapsing forms. DMTs work by altering the immune system to reduce the frequency and severity of relapses, and to slow the accumulation of disability. There are numerous DMTs available, including injectable, oral, and infused medications, each with different mechanisms of action and side effect profiles. Examples include interferon beta, glatiramer acetate, natalizumab, ocrelizumab, and many others. The choice of DMT depends on various factors, including the specific type of MS, disease activity, patient preferences, and potential side effects.
- Corticosteroids: High-dose corticosteroids are often used to treat acute MS relapses. They work by reducing inflammation in the central nervous system, which can help shorten the duration and severity of an attack.
- Symptomatic Treatment: Medications and therapies are also used to manage specific MS symptoms. This can include:
- Muscle relaxants for spasticity
- Medications for fatigue, pain, or bladder dysfunction
- Antidepressants for mood disorders
- Cognitive rehabilitation for memory and thinking problems.
- Rehabilitation Therapies: Physical therapy, occupational therapy, and speech therapy play a crucial role in managing MS. These therapies help individuals maintain mobility, strength, balance, and cognitive function, improving their ability to perform daily activities and enhance their independence.
- Lifestyle Modifications: While not a direct treatment, healthy lifestyle choices can support overall well-being. This includes a balanced diet, regular exercise (as tolerated), stress management, and avoiding smoking.
The field of Multiple Sclerosis research is highly active, with ongoing studies exploring new therapeutic targets, regenerative strategies, and personalized medicine approaches. This continuous progress offers significant hope for even more effective treatments and, eventually, a cure for Multiple Sclerosis.
Living with an MS Diagnosis
Receiving a diagnosis of Multiple Sclerosis can be life-altering, prompting many questions and concerns about the future. However, it's important to remember that an MS diagnosis does not define an individual. With proper management, support, and adaptation, many people with MS lead full and productive lives.
Key aspects of living with an MS diagnosis include:
- Building a Support System: Connecting with family, friends, and support groups can provide emotional comfort, practical assistance, and a sense of community. Sharing experiences with others who understand the challenges of MS can be incredibly valuable.
- Adhering to Treatment Plans: Consistent adherence to prescribed medications and therapies is crucial for managing symptoms and slowing disease progression. Regular follow-ups with neurologists and other healthcare providers ensure that treatment plans are optimized.
- Managing Symptoms Proactively: Learning strategies to cope with common MS symptoms like fatigue, pain, and cognitive changes can significantly improve daily functioning. This might involve energy conservation techniques, pain management strategies, or cognitive exercises.
- Adapting to Changes: MS can be unpredictable, and symptoms may fluctuate. Being adaptable and willing to adjust routines, work environments, or living spaces can help maintain independence and quality of life. This might include using assistive devices or modifying activities.
- Prioritizing Mental Health: Living with a chronic illness can take a toll on mental well-being. Depression and anxiety are common in MS. Seeking counseling, therapy, or engaging in mindfulness practices can be beneficial.
- Advocacy and Awareness: Many individuals with MS become advocates, raising awareness about the disease and supporting research efforts. This can be a powerful way to channel energy and contribute positively to the MS community.
The journey with Multiple Sclerosis is unique for everyone, but a proactive and informed approach to self-management and healthcare partnership can make a significant difference in navigating the challenges and embracing life fully.
Research and the Future Outlook for Multiple Sclerosis
The field of Multiple Sclerosis research is dynamic and constantly evolving, bringing new hope to patients and clinicians alike. Researchers worldwide are dedicated to unraveling the mysteries of MS, from its underlying causes to more effective treatments and, ultimately, a cure. The "Data Kalimat" implicitly acknowledges this progress by mentioning advancements in new drug development.
Current research efforts in Multiple Sclerosis are broadly focused on several key areas:
- Neuroprotection and Neurorepair: A major focus is on developing strategies to protect nerves from damage and to repair damaged myelin. This includes research into remyelination-promoting therapies that could potentially restore lost function.
- Understanding Disease Progression: Studies of the development of progressive Multiple Sclerosis (MS) have focused mostly on brain parenchymal changes, aiming to identify the biological mechanisms driving irreversible disability. This understanding is critical for developing treatments specifically for progressive forms of MS, which have historically been more challenging to treat.
- Biomarkers: Identifying reliable biomarkers that can predict disease course, monitor treatment effectiveness, and diagnose MS earlier is a high priority. These biomarkers could revolutionize personalized medicine in MS.
- Genetic and Environmental Factors: Researchers continue to investigate the complex interplay of genetic predispositions and environmental triggers (like Epstein-Barr virus, vitamin D deficiency, and smoking) that contribute to the development of Multiple Sclerosis.
- Stem Cell Research: Various types of stem cell therapies are being explored for their potential to halt disease progression, promote repair, and alleviate symptoms. While still largely experimental, this area holds significant promise.
- Advanced Imaging Techniques: Innovations in MRI technology allow for more detailed visualization of brain and spinal cord lesions, helping researchers understand disease pathology and treatment effects more precisely.
The collective efforts of scientists, clinicians, and patient advocacy groups are driving rapid progress. While a cure for Multiple Sclerosis remains elusive, the continuous breakthroughs in understanding and treating the disease mean that the future outlook for individuals living with MS is increasingly optimistic, with better long-term outcomes and improved quality of life becoming more achievable.
The Importance of Early Intervention in MS
The timely diagnosis and initiation of treatment are critical factors in managing Multiple Sclerosis effectively. Early intervention can significantly impact the long-term prognosis and quality of life for individuals with MS. This is why understanding the symptoms and seeking medical advice promptly is so important.
Benefits of early intervention in Multiple Sclerosis include:
- Slowing Disease Progression: Disease-modifying therapies (DMTs) are most effective when started early in the disease course, particularly in relapsing forms of MS. By reducing the frequency and severity of relapses and minimizing new lesion formation, early treatment can help slow the accumulation of disability over time.
- Preserving Brain Health: Early treatment helps to reduce brain atrophy (shrinkage) and preserve cognitive function. Research indicates that damage can occur even in the early stages of MS, making early neuroprotection vital.
- Preventing Irreversible Damage: Each relapse can potentially cause new, irreversible damage to the central nervous system. Early intervention aims to minimize these attacks, thereby preventing further neurological deficits.
- Improving Long-Term Outcomes: Studies consistently show that individuals who start DMTs earlier tend to have better long-term outcomes, including reduced disability progression and improved quality of life, compared to those who delay treatment.
- Managing Symptoms More Effectively: Early diagnosis allows for prompt management of symptoms, which can alleviate discomfort and prevent them from becoming chronic or severely debilitating.
As a Mayo Clinic expert explains the basics of Multiple Sclerosis, they often emphasize the importance of early diagnosis and a personalized treatment plan. If you suspect you or a loved one might have symptoms consistent with MS, finding out about Multiple Sclerosis symptoms, causes, prevention, diagnosis, and treatment from reliable sources and consulting a healthcare professional without delay is paramount. A diagnosis of Multiple Sclerosis also involves ongoing monitoring and a collaborative approach between the patient and their medical team to adapt treatment as needed.
Conclusion
Multiple Sclerosis is a complex, chronic neurological condition that impacts countless lives globally. From the breakdown of the protective covering of nerves to the diverse range of symptoms like numbness, weakness, vision changes, and trouble walking, MS presents unique challenges for each individual. While there is currently no cure, the landscape of MS management has been revolutionized by significant advancements in diagnostic tools and disease-modifying therapies. The diagnosis of Multiple Sclerosis is a meticulous process, combining medical history, physical exams, MRIs, and spinal tap results, all aimed at painting a clear picture of the disease's presence and progression.
Understanding the different clinical courses, from the most common relapsing-remitting MS to the more progressive forms, is crucial for tailored treatment and prognosis. The ongoing research into neuroprotection, neurorepair, and progressive MS offers a beacon of hope for future breakthroughs, potentially leading to more effective treatments and even a cure. Living with an MS diagnosis requires a proactive approach, emphasizing early intervention, adherence to treatment plans, and a strong support system. By staying informed, advocating for oneself, and collaborating with healthcare professionals, individuals with Multiple Sclerosis can strive for improved quality of life and better long-term outcomes.
If you or someone you know is experiencing symptoms that might be related to Multiple Sclerosis, we encourage you to seek medical advice from a qualified neurologist. Early diagnosis and intervention are key to managing this condition effectively. Share this article to help spread awareness and understanding about Multiple Sclerosis, and feel free to leave your thoughts or questions in the comments below.
Related Resources:


Detail Author:
- Name : Miss Claudine Walker III
- Username : gabriella.olson
- Email : lulu33@yahoo.com
- Birthdate : 1970-03-16
- Address : 21827 Frank Fords Suite 521 Port Rickview, OK 57311
- Phone : 754.791.8554
- Company : Lemke, Bartoletti and Weissnat
- Job : Lathe Operator
- Bio : Et assumenda praesentium vero ex at. Et eaque doloribus magnam libero quidem iste. Doloribus officia id incidunt quia aut facilis sed.
Socials
linkedin:
- url : https://linkedin.com/in/euna.veum
- username : euna.veum
- bio : Iste sit quidem exercitationem quo.
- followers : 1769
- following : 1409
instagram:
- url : https://instagram.com/euna796
- username : euna796
- bio : Soluta blanditiis assumenda amet praesentium aperiam sed. Quia hic odit molestias.
- followers : 3345
- following : 1450